As treasurer of OSOT, Lesya Dyk contributed the following article to OSOT members via “A Monthly Message from the OSOT Board of Directors” regarding seniors aging in palace which is a current focus of interest as June is National Seniors Month.
Occupational therapy has a significant role to play in helping seniors lead healthy and productive lives. OSOT is working hard to support our members with several initiatives to address the aging population in Canada.
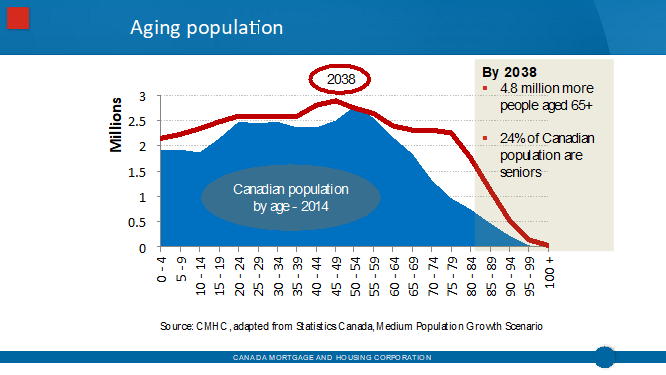
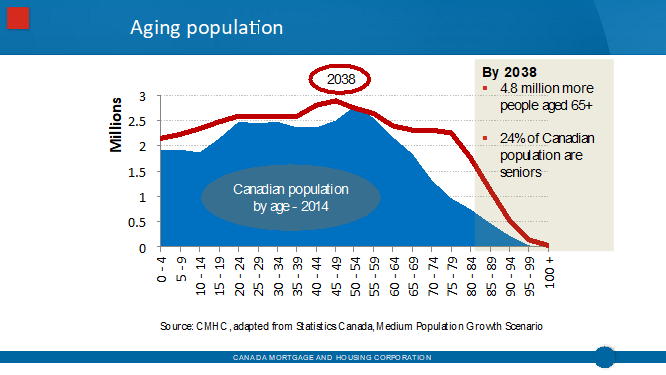
According to Statistics Canada – by 2038, a quarter of our population will be over the age of 65. This will mean that there will be 4.8 million more people over the age of 65 than there are now. The current resources available in health care will not be able to gear up to meet this need.
The reality is that the crisis of how to meet the health needs of the aging population is here. What is certain, there will be more of a role for Occupational Therapy – if we are careful and ready ourselves . This BoardTalk is dedicated to how OSOT is working toward this goal. Consider the following 5 examples of our commitment.
1. Home Modification Canada Steering Committee (HMC)
OSOT was a founding member of the Steering Committee of a consortium called Home Modification Canada (HMC) that was struck by Don Fenn of Caregiver Omnimedia in 2015 to address the “Ageing in Place” issue. While it is clear that a lack of long term care resources will necessitate seniors aging in place, that is, in fact, where research tells us they want to be. HMC was focused on promoting the need to better organize and integrate the home modification marketplace to best meet the needs of that growing aging population who wish to age in place.
In the spring of 2017 HMC made a presentation to the Canadian Home Builders Association (CHBA) with a proposal to develop a multi-faceted national partnership approach that would;
-
support builders/contractors, manufacturers, retailers and set standards, accredit and ensure the quality and value of home modifications
-
coordinate information about existing funding/financing mechanisms for home renovations/modifications
-
support the Canadian Licensing of the CAPS (Certified Ageing in Place Specialist) programme to include a re-written section on Occupational Therapy
-
foster more dynamic public conversations about aging in place and home modifications
-
encourage the application of research and innovation in the fields of smart home technologies, practical products and solutions for home modifications and accessibility
-
support national, provincial and local policy makers to remove barriers, facilitate and incent home modifications for seniors
HMC’s report and recommendations were well received by the CHBA w hich has moved forward to develop a national Home Modification Council. The best news? Our early work and representation and advocacy with HMC has resulted in occupational therapy being the only health profession represented at the Council table!
hich has moved forward to develop a national Home Modification Council. The best news? Our early work and representation and advocacy with HMC has resulted in occupational therapy being the only health profession represented at the Council table!
I have had the pleasure of representing OSOT at the HMC Steering Committee, experiencing the respect and support of our colleague stakeholders in the home modification marketplace, and am delighted to continue this representation at the CHMA Council Table as CAOT now takes on the professional representational role at a national level.
2. OSOT’s Seniors Advisory Council
Two years ago, the Board of Directors engaged a group of members to advise on how best the Society could advance the profession as leaders in seniors health and well-being. As a strategic priority, a focus on seniors has informed initiatives OSOT has undertaken in advocacy, promotion and professional development in virtually all sectors of OT practice, however, our ability to move the needle in terms of leadership and recognition in seniors health is something we wished to advance more fully. Under the chairmanship of Dr. Barry Trentham, our council includes Christie Brenchley, Barbara Cawley, Dr. Catherine Donnelly, Dr. Colleen McGrath, Aaron Yuen and Dr. Briana Zur.
3. A Vision for Enabling Healthy Aging in Ontario – a knowledge mobilization too initiative!
Approving a recommendation and proposal of the Seniors Advisory Council, OSOT is embarking on a new project initiative which aims to promote the evidence-based value of using an occupational lens to respond to the needs of a growing older adult population. Focused on the development of a dynamic website that features modules focused on key life course occupational transitions and profiles the work that occupational therapists are doing and/or could be doing to enable aging well, the project is focused on knowledge mobilization both within and external to the profession.
An enabler of this project has been the successful application of the Society to become a partner of AGE-WELL, Canada’s Aging and Technology Network.
AGE-WELL’s co-funding and resource support to the project both recognizes the value of promoting and enriching occupational therapy as a resource to aging well, but also provides access to knowledge translation resources to support OSOT members who share a practice interest in seniors health and well-being. Watch for our formal launch of this partnership later this month!
Meantime, see our posting for a Post-Doctoral Trainee for a position commencing September 2018 and running to August 2019. This full-time position will take a leadership role in the development, facilitation and evaluation of this knowledge mobilization project. There’s still time to apply! See call for applications.
4. Supporting members practice expertise & leadership relating to seniors health and well-being
Assuming leadership roles in seniors health and well-being requires a ready and informed membership. You have OSOT’s commitment to support your professional development to enable you to position your services to serve the needs of seniors and the health system that supports them.
OSOT’s Conference 2018, ADVANCE! Journey to Excellence,
provides but one opportunity to get involved, participate and learn. This year we will host a professional issues/leadership forum focused on advancing our profession’s roles in seniors health and well-being – plan to be a part! Reserve the Conference dates – October 19 – 20, 2018 now!
 The Society continues to look at opportunities to host webinars and workshops to give our membership the tools that they need to work in this arena. Watch for the 2018 – 19 PD Program of Events and check out our listing of Archived Webinars that can support your practice in this area.
The Society continues to look at opportunities to host webinars and workshops to give our membership the tools that they need to work in this arena. Watch for the 2018 – 19 PD Program of Events and check out our listing of Archived Webinars that can support your practice in this area.
5. Advocacy to position occupational therapy in seniors health services
OSOT continues to advocate for occupational therapy services for seniors across Ontario’s health care system. Our advocacy document, Occupational Therapy Can Help; challenges of an aging population has been shared broadly with government and amongst MPPs at our annual MPP Luncheon. There are so many ways that OTs can contribute and make meaningful differences to seniors health and quality of life, however, Ontarians need increased access to OT services! We have active advocacy and government relations strategies relating to:
As the OSOT Board puts the finishing touches on our new Strategic Plan, we will reveal how we will continue to advance work that supports our members, senior citizen clients and their families to ask for Occupational Therapy Services… and to access them! Stay tuned!
 Lesya Dyk,
Lesya Dyk,
President and Director of Clinical Service,
LDOT Services.
360 Queenston Rd., 2nd Floor, Unit# 3
Hamilton, ON
L8K 1H9
Hamilton: 905-481-1122
Toronto: 416-907-6287
Fax: 905-481-2550
Email: info@ldot.ca





 hich has moved forward to develop a national Home Modification Council. The best news? Our early work and representation and advocacy with HMC has resulted in occupational therapy being the only health profession represented at the Council table!
hich has moved forward to develop a national Home Modification Council. The best news? Our early work and representation and advocacy with HMC has resulted in occupational therapy being the only health profession represented at the Council table!

 The Society continues to look at opportunities to host webinars and workshops to give our membership the tools that they need to work in this arena. Watch for the 2018 – 19 PD Program of Events and check out our listing of
The Society continues to look at opportunities to host webinars and workshops to give our membership the tools that they need to work in this arena. Watch for the 2018 – 19 PD Program of Events and check out our listing of 









